The Utilization Management (UM) healthcare market faces challenges such as administrative burdens in prior authorization and inconsistent clinical criteria, causing delays and inefficiencies. To overcome these issues, payers are partnering with specialized UM service providers, integrating generative AI, automation, and clinical expertise to streamline workflows and enhance decision-making. Payers are increasingly adopting outcome-based pricing models, linking payments to patient health outcomes rather than service volume.
These collaborations improve operational efficiency, accelerate care delivery, reduce costs, and ensure high-quality, evidence-based patient care, ultimately boosting provider alignment and patient satisfaction.
-
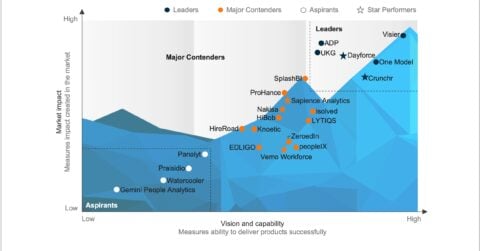
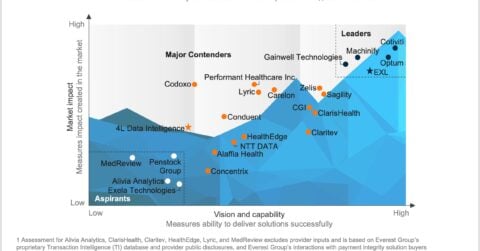
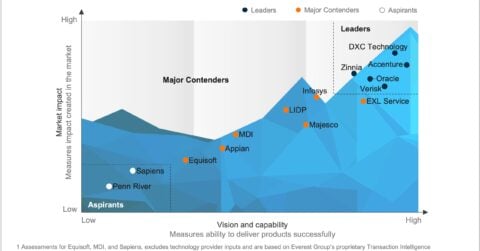
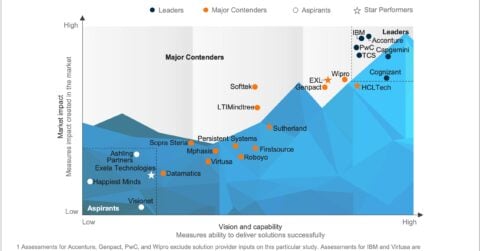
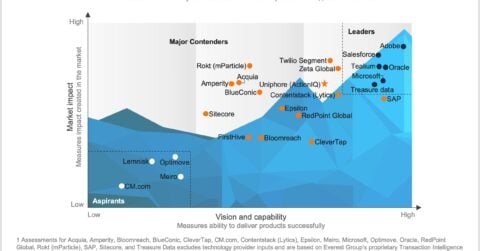
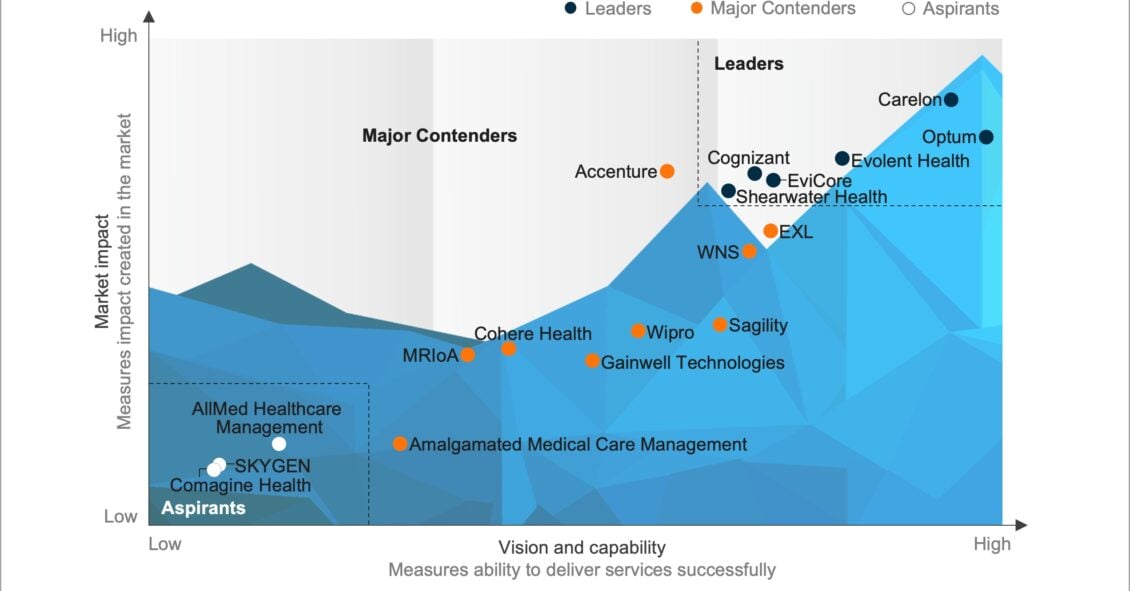
Utilization Management (UM) Operations PEAK Matrix® Assessment 2025
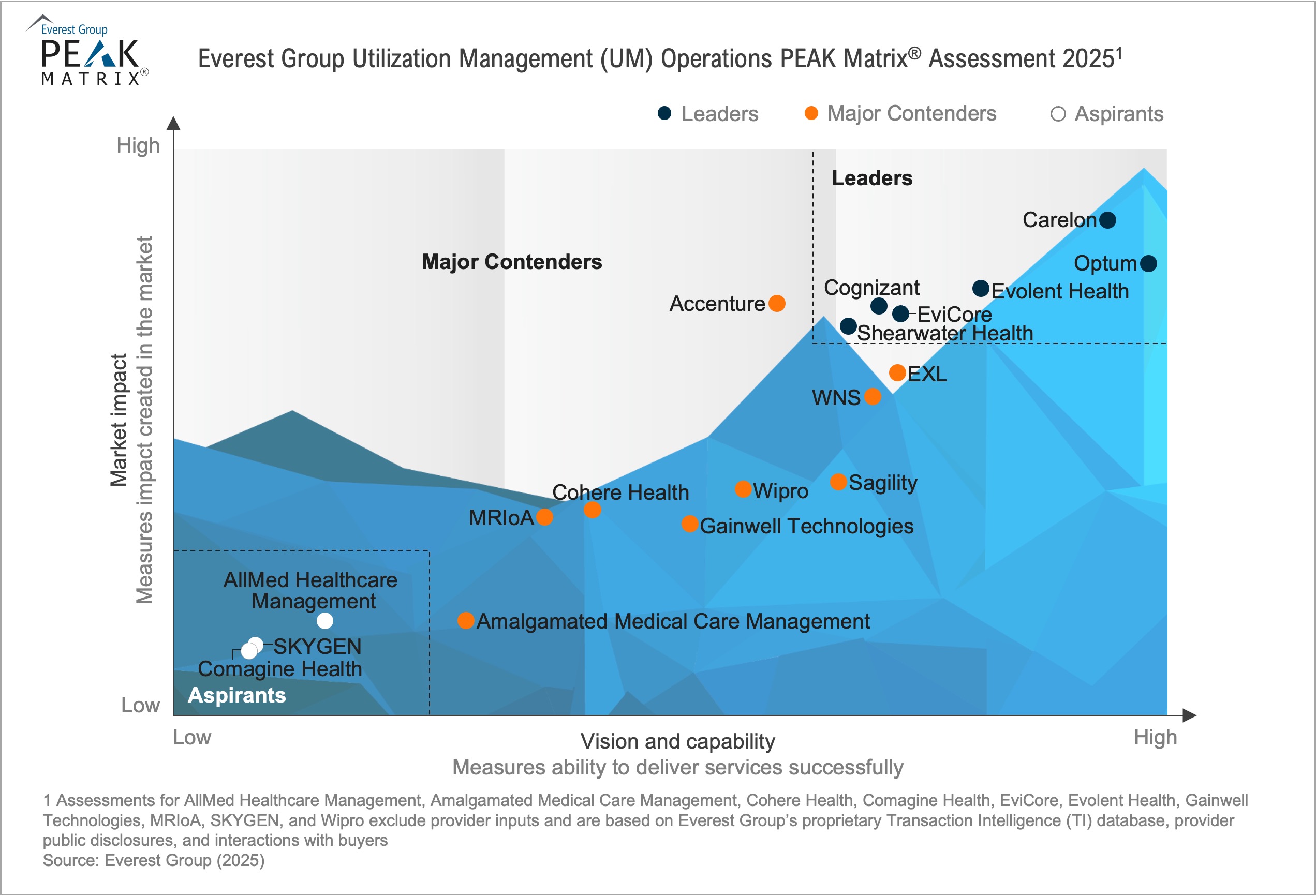
In this report, we analyze 18 providers featured on the Utilization Management Operations PEAK Matrix®. The report positions providers relative to each other and evaluates their strengths and limitations. The study will enable healthcare payers to identify suitable providers to transform their business processes and differentiate themselves from competitors.
Scope
- Industry: healthcare
- Geography: US
- This assessment is based on Everest Group’s annual RFI process for the calendar year 2024, interactions with leading UM operations providers, client reference checks, and an ongoing analysis of the UM operations market
Contents
In this report, we examine:
- The Utilization Management Operations PEAK Matrix® Assessment 2025
- The UM operations provider landscape
- Providers’ key strengths and limitations
READ ON
What is the PEAK Matrix®?
The PEAK Matrix® provides an objective, data-driven assessment of service and technology providers based on their overall capability and market impact across different global services markets, classifying them into three categories: Leaders, Major Contenders, and Aspirants.